Outsource prior authorization services
Pre-authorizations (PAs) are a very labor-intensive task for healthcare providers, their staff, and patients. Prior authorization is a process by which healthcare providers must be eligible for payment coverage. This is done by obtaining advanced approval from a health plan before a specific service is delivered to a patient. According to the American Medical Association (AMA), prior authorization is overused, and existing processes present significant administrative and clinical concerns. Outsourcing your prior authorizations process can help your practice focus on patient care. It will also allow a trusted partner to manage the process with high quality standards while relieving your staff of the administrative burden.
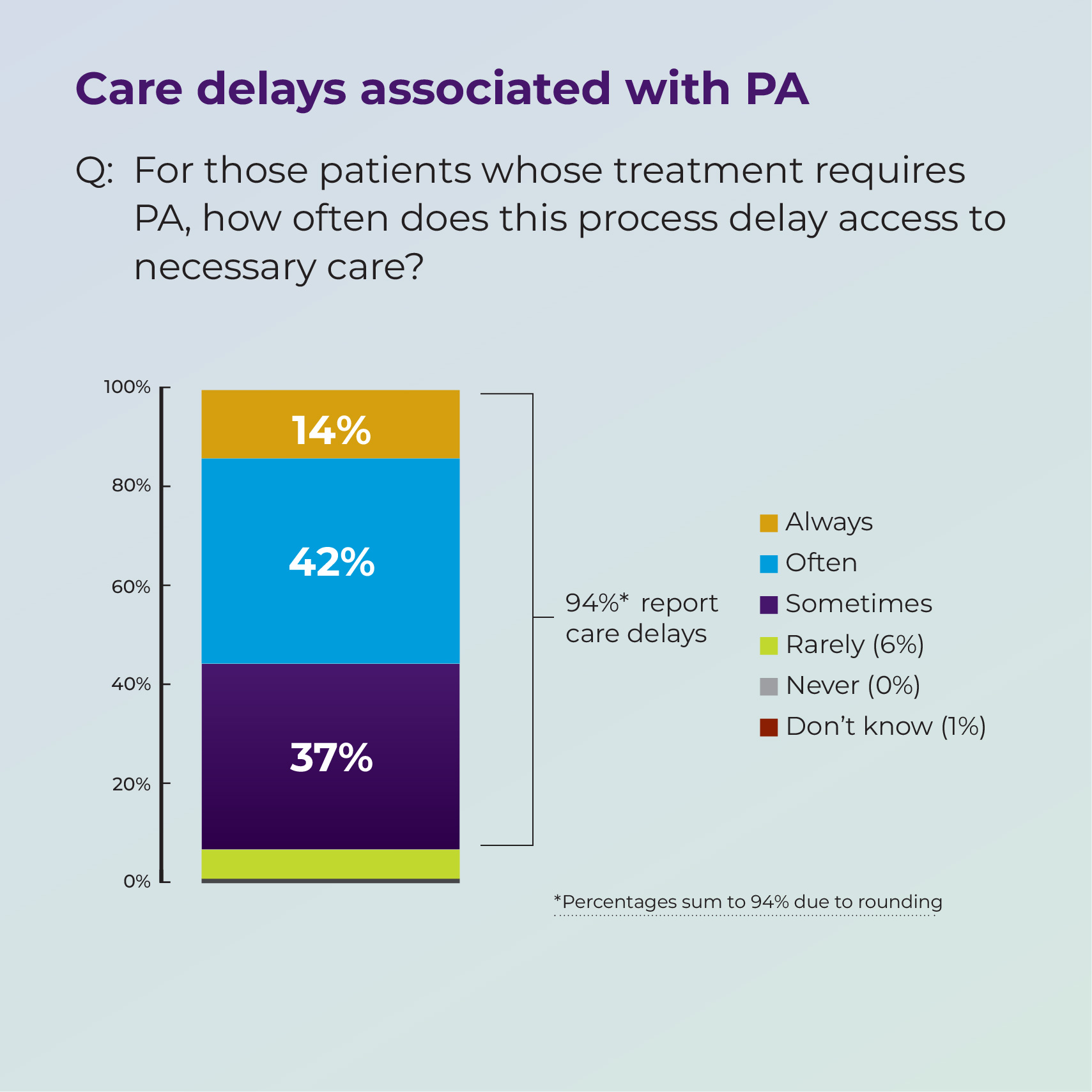
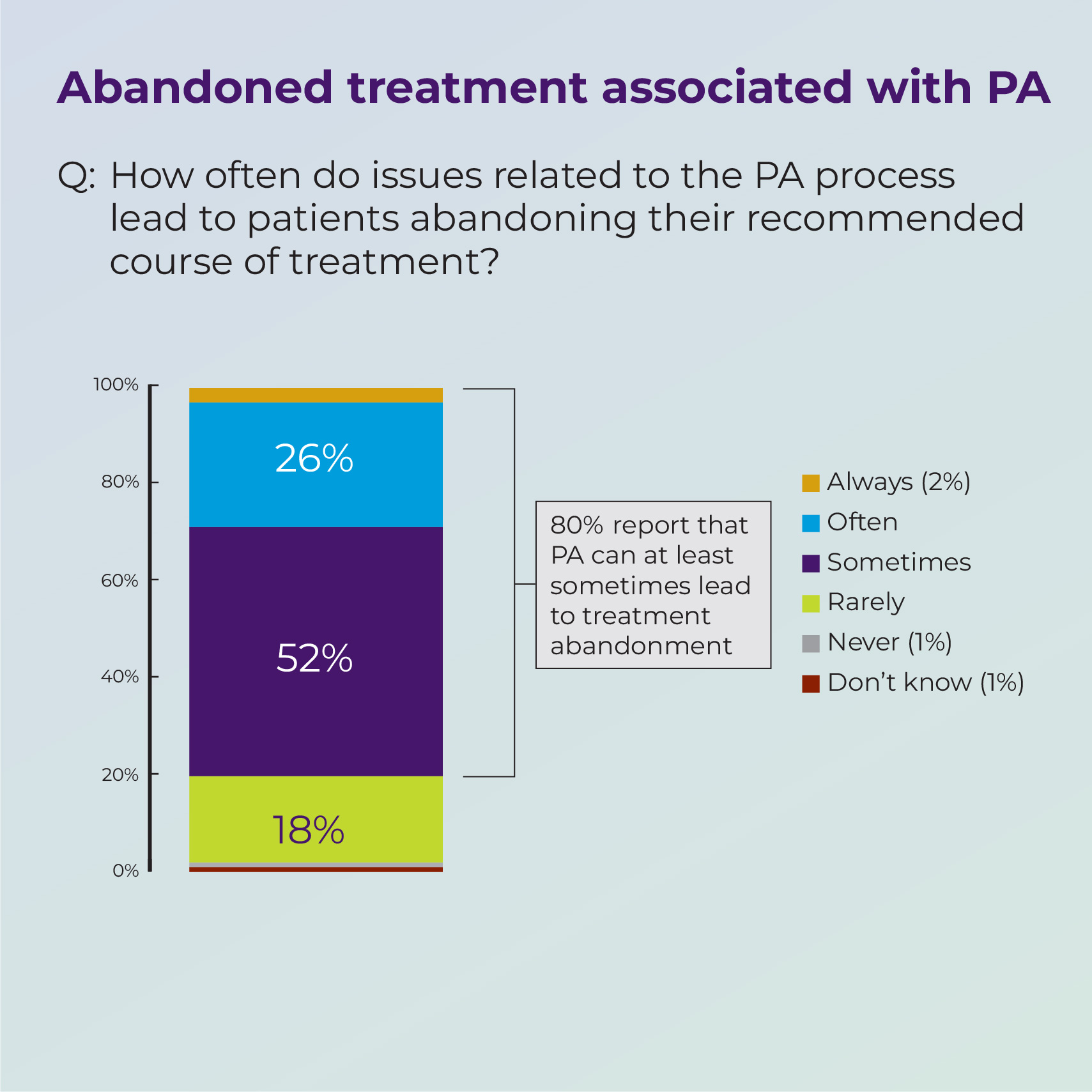
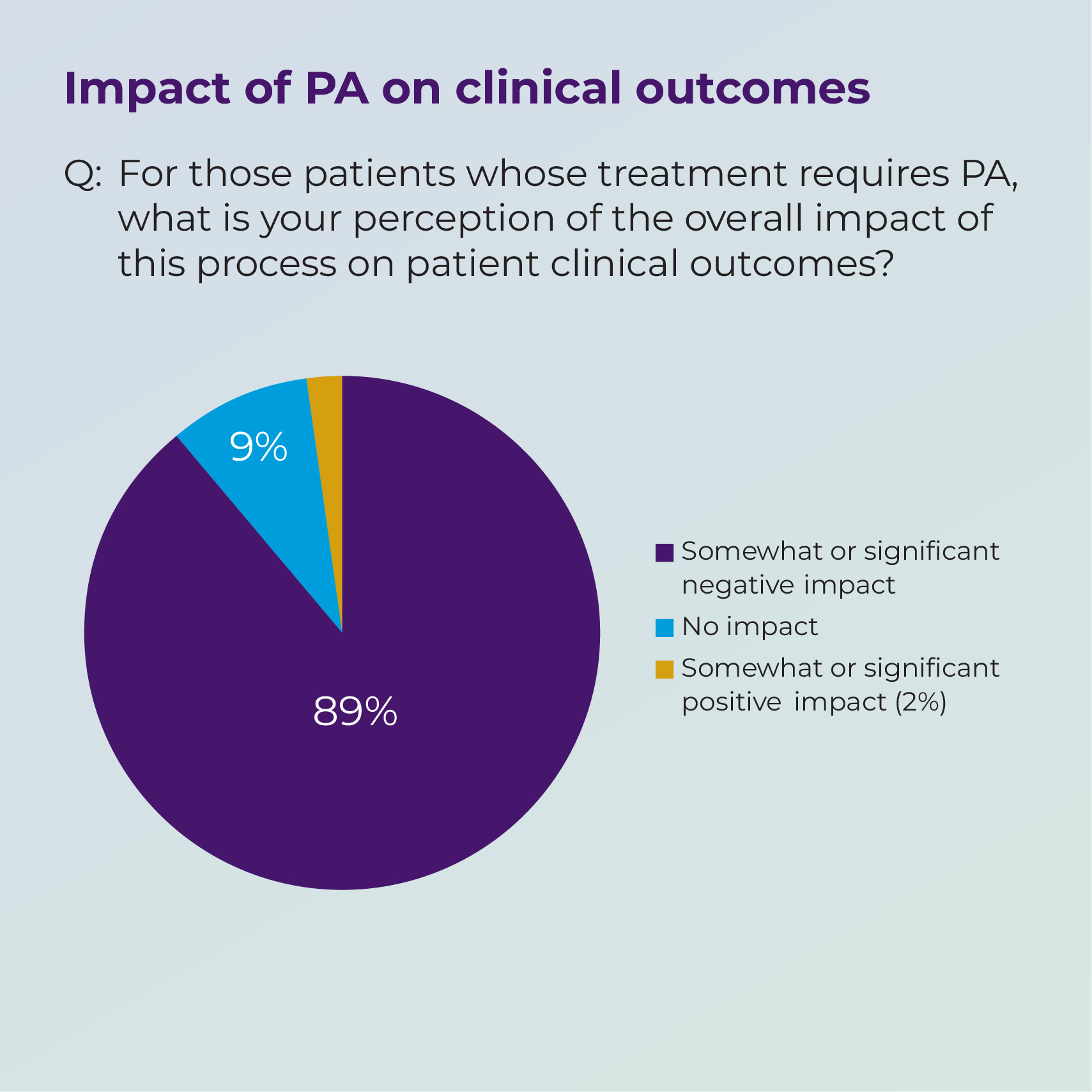
Source : https://www.ama-assn.org/system/files/prior-authorization-survey.pdf
Let us know how we can help!
MedScript offers Prior Authorization, our optimized Virtual Office solution that helps with prior authorization or pre-certification of services you are rendering, depending on your medical practice needs. We can do the work to obtain the precertification/prior authorization of services for a patient. If we have all proper documentation from the practice and provider, we can process it.
Proper documentation for this process consists of a completed and signed medical record with:
- the test or procedure order listed along with the body part.
- CPT code or specific procedure ordered.
- the ICD10 code.
- any previous treatments or medications tried.
Outsourcing your prior authorizations process helps medical practices focus on patient care and allows us to gather, filter, report, and manage your process with an unbiased approach. We also stay updated on changing government regulations, so your practice doesn´t have to worry about authorization compliance issues.
 Reduce Denials
Reduce Denials